Session Abstract – PMWC 2018 Silicon Valley
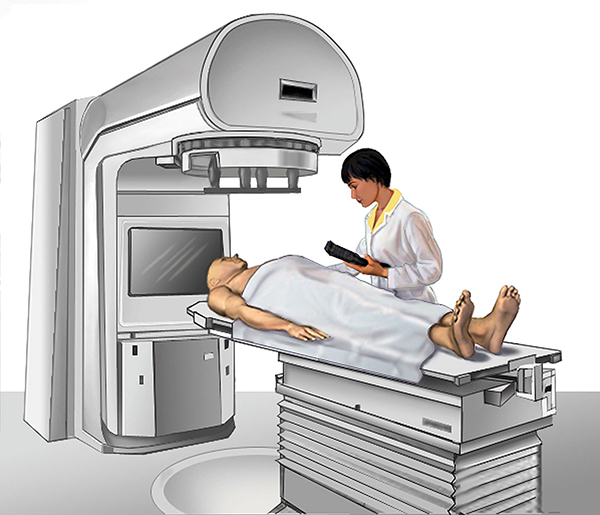
Session Synopsis: Recent advancements in engineering, molecular biology, imaging and machine learning are posed to revolutionize radiotherapy and improve the outcome in cancer patients. We will review the growing body of evidence on radiation technology development, imaging-based radiotherapy, prognostic biomarkers of radiosensitivity/radioresistance, and the benefits of combining immunooncology with radiotherapy.
Session Chair Profile
M.D., Professor and Chair, Stanford University School of Medicine, Department of Radiation Oncology
Biography
Quynh-Thu Le, FACR, FASTRO holds the Katharine Dexter McCormick & Stanley McCormick Memorial Professorship at Stanford University. She is also the chair of the Head and Neck Cancer Committee of NRG Oncology. Her research focuses on head and neck cancer (HNC), specifically in the area of tumor hypoxia and salivary gland regeneration. On the clinical side, she has led multicenter phase II and III clinical trials, testing the addition of novel drugs as either radiosensitizer or radioprotector with chemoradiotherapy in HNC.
Speaker Profile
M.D., Ph.D., Assistant Professor, Stanford University School of Medicine
Biography
Maximilian Diehn received his Bachelor’s Degree in Biochemical Sciences from Harvard College and his M.D./Ph.D. in Biophysics from Stanford University. He is a board certified Radiation Oncologist and specializes in the treatment of lung cancers. Dr. Diehn’s current research program spans laboratory, translational, and clinical studies. His areas of interest include cancer genomics, stem cell biology, and lung cancer biology. His work has been recognized with a variety of awards, including the V Foundation Scholar Award, the Sidney Kimmel Scholar Award, the Doris Duke Clinical Scientist Development Award, and the NIH Director’s New Innovator Award. His group has developed an ultra sensitive and specific method for detection of circulating tumor DNA called CAPP-Seq. Current work is focused on applying CAPP-Seq to a range of clinical contexts, with an emphasis on tumor heterogeneity and minimal residual disease.
Talk
Applications of Circulating Tumor DNA to Guide Treatment Decisions
Circulating tumor DNA (ctDNA) represents a promising biomarker for sensitive, specific, and dynamic detection of disease burden in cancer patients. In this presentation I will discusses using ctDNA as a cancer biomarker, with a particular emphasis on potential applications in patients treated with radiotherapy.
Speaker Profile
Ph.D., Jacob Haimson Professor, Stanford University; Director of Medical Physics Division of Radiation Oncology Department at Stanford
Biography
Dr. Xing holds affiliate faculty positions in Departments of Electric Engineering (courtesy), Medical Informatics, Bio-X and Molecular Imaging Program at Stanford. Dr. Xing obtained his PhD in Physics from the Johns Hopkins and received his Medical Physics training at the University of Chicago. His research has been focused on artificial intelligence in medicine, inverse treatment planning, tomographic image reconstruction, CT, and PET imaging instrumentations, image guided interventions, nanomedicine, and applications of molecular imaging in radiation oncology. Dr. Xing is an author on more than 300 peer-reviewed publications, a co-inventor on many issued and pending patents, and a co-investigator or principal investigator on numerous NIH, DOD, NSF, ACS grants and projects from other funding agencies and corporates. He and his lab members have received numerous awards from ACS, AAPM, ASTRO, WMIC, and RSNA in the past decade. Dr. Xing is on the editorial boards of a number of journals in radiation physics and medical imaging.
Talk
Technological Advances in Precision Radiation Medicine
Radiation therapy is the original precision targeted cancer treatment. Major advances in medical imaging and exquisite radiation dose sculpting technologies have dramatically increased physical precision of radiation therapy. This presentation summarizes current state-of-the-art and emerging advances leading to new levels of physical and biological precision in cancer radiation therapy.
Speaker Profile
M.D., Ph.D., Associate Professor, University of Pennsylvania
Biography
Dr. Minn’s research is focused on how cancers acquire treatment resistance and how resistance can be overcome. His lab has identified pattern recognition receptors (PRR) and interferon (IFN) pathways across multiple cancer types. In the context of cancer, these pathways orchestrate tumor progression, response to conventional or immunotherapies, and immunosuppression. The lab is investigating how PRR/IFN signaling is activated in cancer, both cell intrinsically and through the tumor microenvironment. These PRR/IFN pathways can be therapeutically exploited to modulate the immune system. One way is through activation of the DNA damage response. An overarching goal is to translate mechanistic findings to inform clinical trial design. Dr. Minn is an Associate Professor in the Department of Radiation Oncology and Abramson Family Cancer Research Institute at the University of Pennsylvania. He received his MD and PhD from the University of Chicago and his medical and post-doctoral training at Memorial Sloan Kettering Cancer Center.
Talk
Overcoming Resistance to Immune Checkpoint Blockade
Although immune checkpoint blockade (ICB) for cancer can result in impressive responses, most solid tumors either do not respond or relapse. We will discuss two general strategies to improve ICB efficacy: 1) Discovery and targeting of resistance mechanisms, and 2) Activating pattern recognition receptors through radiation and damage-associated molecular patterns.
Speaker Profile
M.D., Ph.D., Associate Professor, Stanford University

Biography
Dr. Loo is a physician-scientist Radiation Oncologist and Bioengineer who leads the Thoracic Radiation Oncology program at Stanford Cancer Institute. His clinical specialties are state-of-the-art radiation therapy for lung/thoracic cancers, including stereotactic ablative radiotherapy (SABR) and 4-D image-guided radiation therapy for lung tumors. His research is in clinical trials and implementation of new treatment techniques for lung cancer, development of new medical imaging methods for measuring organ function and predicting response to cancer treatment, and development of next generation radiation treatment technologies and studying their unique biological effects. Dr. Loo is a recognized expert in thoracic cancers serving on multiple national committees (including as writing member, chair, or vice-chair) that publish clinical guidelines on the treatment of lung cancer and other thoracic malignancies, including the National Comprehensive Cancer Network (NCCN), American College of Radiology (ACR), and American Society of Radiation Oncology (ASTRO). Dr. Loo received his MD from University of California, Davis and his PhD in Bioengineering from University of California, San Francisco and Berkeley. He completed his Radiation Oncology residency training at Stanford University where he is now Associate Professor of Radiation Oncology. He is certified by the American Board of Radiology in Radiation Oncology.
Talk
Technological Advances in Precision Radiation Medicine
Radiation therapy is the original precision targeted cancer treatment. Major advances in medical imaging and exquisite radiation dose sculpting technologies have dramatically increased physical precision of radiation therapy. This presentation summarizes current state-of-the-art and emerging advances leading to new levels of physical and biological precision in cancer radiation therapy.